Wobbly, sore ankle? It’s often a lateral ligament injury or chronic instability — here’s how we fix it
- 지수 이
- Aug 14, 2025
- 2 min read







Wobbly, sore ankle? It’s often a lateral ligament injury or chronic instability — here’s how we fix it
At a glance
What you feel | Where it hurts | Why it happens | First helpful step |
“Gives way”, sharp pain, swelling after a twist | Outer ankle (ATFL/CFL), sometimes front | Inversion sprain, over‑pronation, repeated shoe friction, under‑rehabbed sprain | Short‑term support & load reduction → book an assessment for a tendon‑safe, stability‑focused plan |
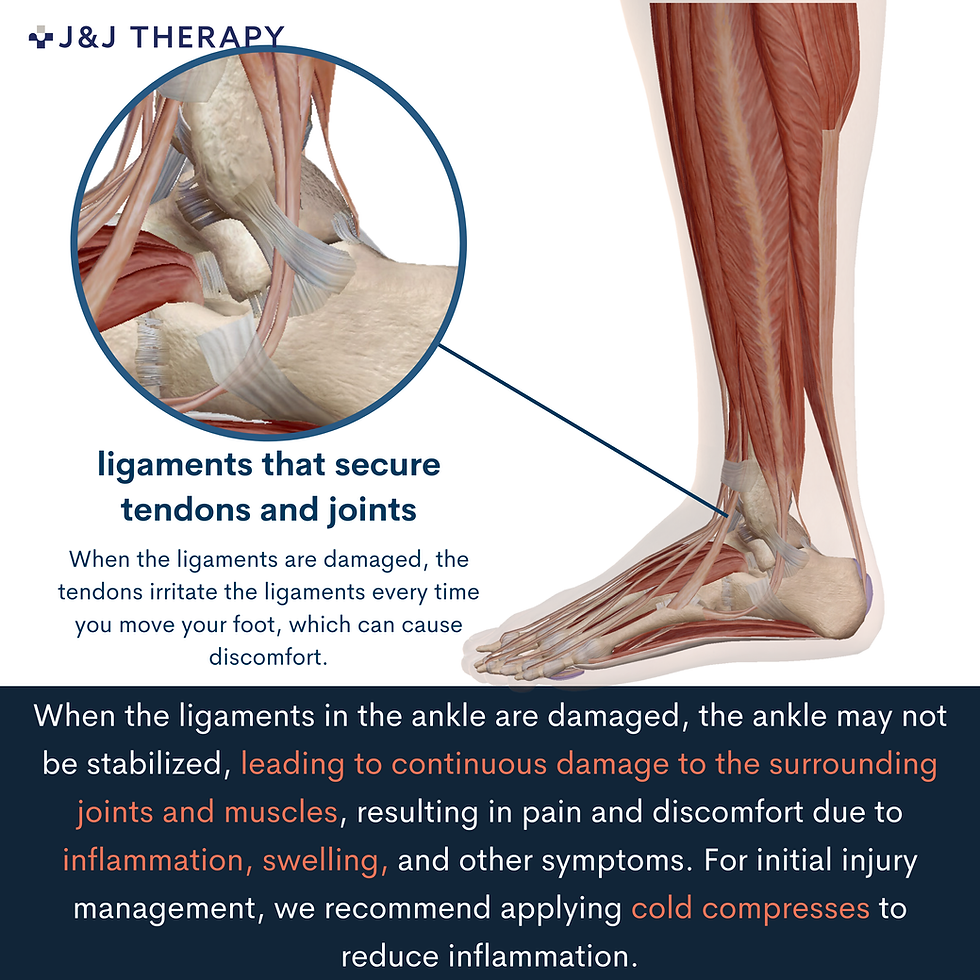
What do ankle ligaments do?
Ligaments connect bone to bone and keep joints stable. The outer ankle relies on three ligaments—ATFL, CFL, PTFL—to stop the ankle sliding forward and over‑rolling. Because ligaments have limited blood supply, recovery can be slow without the right plan.
Quick self‑check
Checklist | Yes/No |
Feeling of instability or “giving way” | |
Pain with walking, stairs or uneven ground | |
Swelling or stiffness around the outer ankle | |
Recurrent sprains or fear of twisting again |
Seek urgent care if you cannot bear weight after injury, have severe deformity, numbness/tingling, or night pain with fever.
Why it flares up / lingers
Sudden inversion sprain; poor footwear or laces rubbing the ligaments
Returning to running/sport too quickly after a sprain
Poor balance/ankle control; over‑pronation and tight calves
Our treatment plan (clear phases)
Phase & goal | What we use at J&J Therapy | What it does |
Calm inflammation | Shockwave therapy (for stubborn/chronic pain), Ultrasound therapy, short‑term taping or brace | Settles pain, stimulates local healing, reduces shear on ligaments |
Ease pain | Electrical therapy (TENS/EMS) | Short‑term analgesia so you can move & sleep |
Release overload | Therapeutic massage to peroneals, calf & foot; ankle mobilisation | Reduces tissue tension & joint guarding |
Restore stability | Corrective exercise education: isometrics → balance (single‑leg, wobble surface) → strength (peroneals/calf/hip) → return‑to‑run plan | Rebuilds ligament support & prevents recurrence |
If swelling present | Lymphatic massage | Assists fluid movement & comfort |
What a session looks like
Step | What happens | Your takeaway |
1. Consult & assess | We confirm which ligament is involved and rule out fractures/nerve issues | Clear diagnosis & goals |
2. Hands‑on & device care | Corrective/therapeutic massage + shockwave where indicated | Pain down, confidence up |
3. Your mini programme | 3–5‑minute home routine (+ footwear & terrain tips) | Control symptoms between visits |
Home tips until you visit
First 24–48 hrs of a flare: cold compress 10–15 min, 2–3×/day
Supported walking (taping/brace) on uneven ground; avoid sudden cutting/plyometrics
Isometrics: push the foot gently outwards into a wall/strap, 5×10 s, pain‑free
Daily balance: stand on one leg (eyes open → closed) 30–45 s, 2–3 sets
Lace shoes snugly and choose a supportive trainer
Ready to trust your ankle again?
Most clients feel meaningful relief within 3–6 sessions and leave with a simple, personalised stability plan. Book your assessment and get back to walking, work and sport with confidence.



Comments