Calf Pain When Walking? It Might Be ‘Tennis Leg’—What It Is & How We Treat It
- 지수 이
- Aug 14, 2025
- 3 min read








Calf Pain When Walking? It Might Be ‘Tennis Leg’—What It Is & How We Treat It
What is happening in your calf?
Your calf is mainly the gastrocnemius (top, power muscle) and soleus (deeper, endurance). A sudden push‑off, change of direction or an explosive jump can over‑stretch the gastrocnemius and create a partial tear—often called tennis leg.
Quick self‑check
Did it feel like being hit by a stone/ball?
Did you hear or feel a pop with sharp pain?
Is it painful to push off the toes, walk or jog?
Is there swelling or bruising around the calf or ankle?
If these sound familiar, you may have tennis leg.
First 48 hours: Do vs Don’t
Do | Don’t |
Relative rest (avoid painful push‑off) | Don’t “test” sprint or jump |
Ice 10–15 min, 3–5×/day | No aggressive stretching |
Compression bandage/sleeve | Avoid deep tissue massage early on |
Elevate leg when resting | Don’t ignore rapidly worsening swelling, warmth or colour change |
Seek urgent care (A&E/111) if you have calf swelling with warmth/redness, unexplained breathlessness or chest pain – these can be signs of DVT or other medical emergencies.
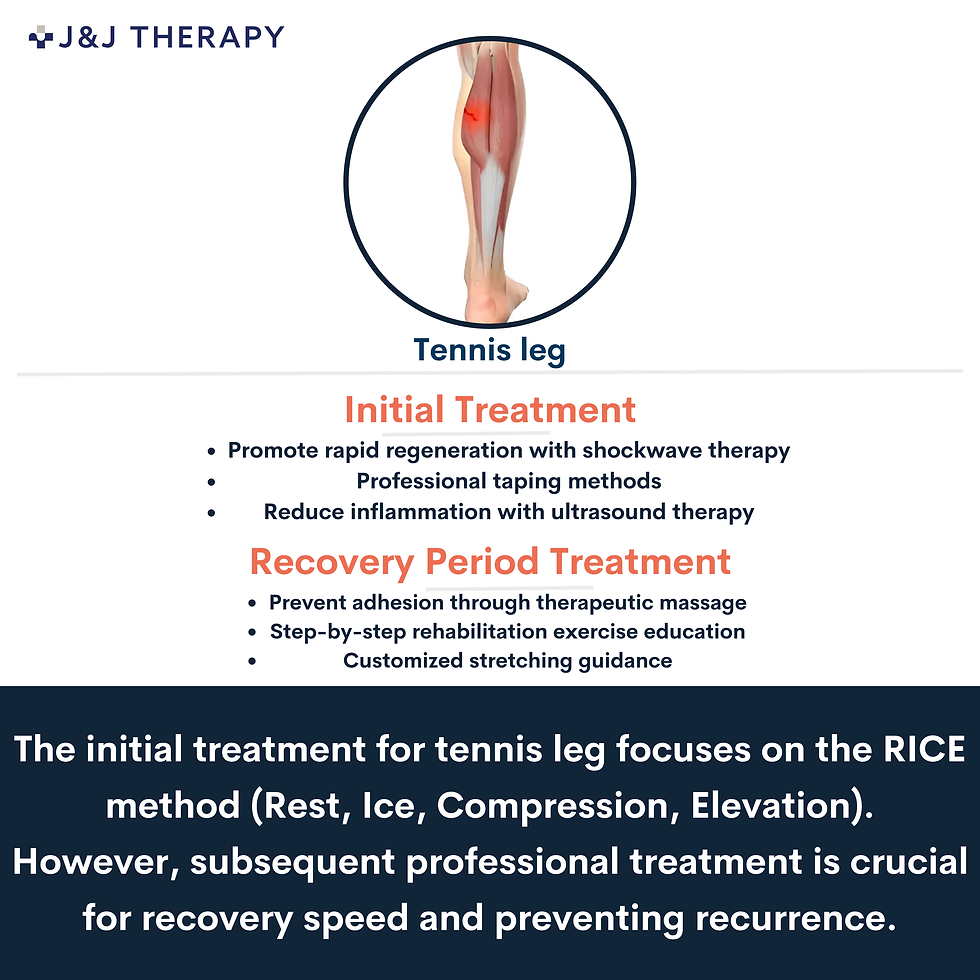
How J&J Therapy treats tennis leg
We combine hands‑on care and technology to reduce pain, speed healing and prevent re‑injury.
Stage | Your goals | Recommended care at J&J |
Acute (Days 1–7) | Calm pain & swelling | Shockwave therapy (clinician‑set dosage), ultrasound therapy to reduce inflammation, gentle TENS for pain relief, professional taping to support the calf, lymphatic drainage massage for swelling control. |
Sub‑acute (Weeks 2–3) | Restore movement | Therapeutic massage (targeted, non‑aggressive) to reduce adhesions; progressive isometric → isotonic calf loading; gait re‑training. |
Rehab (Weeks 3–6+) | Rebuild strength & prevent relapse | Progressive heel‑raise programme, balance work, return‑to‑run plan; bespoke stretching and mobility; sport‑specific drills. |
Why shockwave here? It’s a non‑invasive modality used by our therapists to tackle inflammation/adhesions, improve local circulation and support tissue regeneration when dosed appropriately in your plan.
Expected recovery (guide only)
Mild tear: ~2–3 weeks
Moderate: ~4–6 weeks
Severe/large partial: 6–12+ weeks with structured rehab
Every case is different—your therapist will tailor loading and timelines to your progress.
When to seek medical assessment urgently
Sudden inability to push off or marked weakness (consider Achilles rupture—urgent imaging).
Calf swelling, warmth, redness, disproportionate pain, or shortness of breath/chest pain (possible DVT/PE—A&E).
Severe pain that doesn’t settle at rest or overnight.
Book an assessment
WhatsApp 07882 943540 (main line) / Text 07935 869938 (EN & KR)
Email info@jjwellcare.com
J&J Therapy – Therapeutic Massage & Physio (UK).We have 7+ years of clinical experience and provide care in English & Korean.
FAQs
1) Is tennis leg the same as a cramp?No. A cramp eases within minutes. Tennis leg causes a sharp pain (often with a “pop”), swelling/bruising and pain on push‑off.
2) Can I stretch it straight away?Avoid strong stretching for the first few days. Start gentle range‑of‑motion and progressions as advised by your therapist.
3) Do I need imaging?Many partial tears are diagnosed clinically. Imaging is considered if symptoms are severe, atypical, or not improving.
4) When can I run again?When walking is pain‑free, you have near‑full calf strength and can perform controlled heel raises without pain. We’ll phase a graded return‑to‑run.
5) Will massage help?Yes—therapeutic massage in the sub‑acute stage helps reduce adhesions and restore glide. Very deep work is avoided in the first few days.
Medical disclaimer: This article is educational and not a substitute for personalised medical advice. If in doubt, consult your GP or attend A&E.



Comments